CDC is aware of reports of increased numbers of babies born with microcephaly (smaller than expected head size) in Brazil. The Ministry of Health (MOH) of Brazil is concerned about a possible association between the Zika virus outbreak and increased numbers of babies born with microcephaly.
There are many causes of microcephaly There are many causes of microcephaly in babies (e.g., infections a mother can get during pregnancy, genetic abnormalities, exposure to toxic substances during pregnancy).
Because of this, it will take time to determine the cause of microcephaly for the cases being reported in Brazil. Microcephaly in Brazil Starting in October 2015, the Brazilian MOH received reports of an increase in the number of babies being born with microcephaly.
The number of microcephaly cases are roughly 10 times higher than what the country normally sees in a year.
Some samples from babies with microcephaly have tested positive for Zika virus infection but several affected babies have also tested negative using the same test.
CDC is not aware of any published reports of increased numbers of microcephaly associated with other similar viral (i.e. flaviviral) diseases transmitted by mosquitoes.
Zika virus in Brazil
Brazil reported its first case of Zika virus disease in May 2015. Since then, the virus has spread and has caused infections in many Brazilian states and other countries in Latin America.
The association of Zika virus infection and microcephaly and is still under investigation. If you are pregnant and traveling to Brazil or other countries in Latin America: CDC recommends that all people, especially pregnant women, who are traveling to Brazil and other areas in Latin America, should take precautions to avoid mosquito bites to reduce their risk of infection with Zika virus and other mosquito-borne viruses such as dengue and chikungunya. For more information: Zika virus: What you need to know Mosquito bite prevention for travelers Traveling? Get country-specific travel recommendations: www.cdc.gov/travel Zika virus: Pan American Health Organization
http://www.cdc.gov/zika/pdfs/possible-association-between-zika-virus-and-microcephaly.pdf
Zika virus is spread to people through mosquito bites. The most common symptoms of Zika virus disease are fever, rash, joint pain, and conjunctivitis (red eyes). The illness is usually mild with symptoms lasting from several days to a week. Severe disease requiring hospitalization is uncommon. A possible link[PDF - 1 page] between Zika virus infection in pregnant women and subsequent birth defects is being investigated in Brazil.
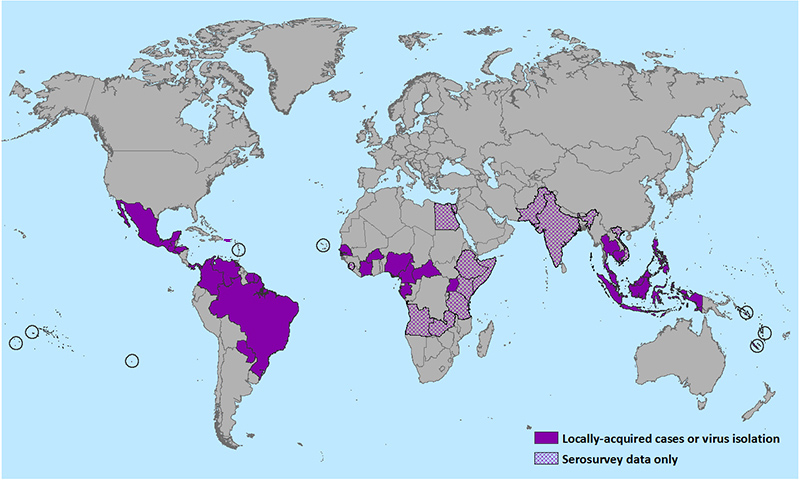
Outbreaks of Zika have occurred in areas of Africa, Southeast Asia, the Pacific Islands, and the Americas. Because the Aedes species mosquitoes that spread Zika virus are found throughout the world, it is likely that outbreaks will spread to new countries. In December 2015, Puerto Rico reported its first confirmed Zika virus case. Locally transmitted Zika has not been reported elsewhere in the United States, but cases of Zika have been reported in returning travelers.
There is no vaccine to prevent or medicine to treat Zika. Travelers can protect themselves from this disease by taking steps to prevent mosquito bites. When traveling to countries where Zika virus (see map) or other viruses spread by mosquitoes have been reported, use insect repellent, wear long sleeves and pants, and stay in places with air conditioning or that use window and door screens.
Prevention
Symptoms
- About 1 in 5 people infected with Zika virus become ill (i.e., develop Zika).
- The most common symptoms of Zika are fever, rash, joint pain, or conjunctivitis (red eyes). Other symptoms include muscle pain, headache, pain behind the eyes, and vomiting.
- The illness is usually mild with symptoms lasting for several days to a week.
- Severe disease requiring hospitalization is uncommon.
- Deaths due to Zika have not been reported.
Diagnosis
- The symptoms of Zika are similar to those of dengue and chikungunya, which are diseases caused by other viruses spread by the same type of mosquitoes.
- See your healthcare provider if you develop the symptoms described above.
- If you have recently traveled, tell your healthcare provider.
- Your healthcare provider may order blood tests to look for Zika or other similar viruses like dengue or chikungunya viruses.
Treatment
- There is no medicine to treat Zika.
- Treat the symptoms:
- Get plenty of rest
- Drink fluids to prevent dehydration
- Take medicines, such as acetaminophen or paracetamol, to relieve fever and pain
- Aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided until dengue can be ruled out to reduce the risk of hemorrhage
More detailed information can be found on CDC’s Zika virus web page for healthcare providers
Geographic Distribution
Outbreaks of Zika virus disease (or Zika) previously have been reported in tropical Africa, Southeast Asia, and the Pacific Islands. Zika virus likely will continue to spread to new areas. In May 2015, the Pan American Health Organization (PAHO) issued an alert regarding the first confirmed Zika virus infections in Brazil.
In December 2015, Puerto Rico reported its first confirmed Zika virus case. Locally-transmitted Zika virus has not been reported elsewhere in the United States, but cases of Zika have been reported in returning travelers. With the recent outbreaks in the Pacific Islands and South America, the number of Zika cases among travelers visiting or returning to the United States will likely increase. These imported cases may result in local spread of the virus in some areas of the United States.
Countries that have past or current evidence of Zika virus transmission (as of December 2015)
For Health Care Providers: Clinical Evaluation & Disease
Zika virus is a single-stranded RNA virus of the Flaviviridae family, genus Flavivirus. Zika virus is transmitted to humans primarily through the bite of an infected Aedes species mosquito. The mosquito vectors typically breed in domestic water-holding containers; they are aggressive daytime biters and feed both indoors and outdoors near dwellings. Nonhuman and human primates are likely the main reservoirs of the virus, and anthroponotic (human-to-vector-to-human) transmission occurs during outbreaks.
Perinatal and possible sexual transmission has also been reported. Transfusion-associated transmission is possible as Zika virus RNA has been identified in asymptomatic blood donors during an ongoing outbreak.
Clinical Signs & Symptoms
About 1 in 5 people infected with Zika virus become symptomatic. Characteristic clinical findings are acute onset of fever with maculopapular rash, arthralgia, or conjunctivitis. Other commonly reported symptoms include myalgia, headache, retro-orbital pain and vomiting. Clinical illness is usually mild with symptoms lasting for several days to a week. Severe disease requiring hospitalization is uncommon and case fatality is low. There is one case report of Guillain-Barre syndrome in a patient with probable Zika virus infection.
Diagnosis & Reporting
Based on the typical clinical features, the differential diagnosis for Zika virus infection is broad. In addition to dengue, other considerations include leptospirosis, malaria, rickettsia, group A streptococcus, rubella, measles, and parvovirus, enterovirus, adenovirus, and alphavirus infections (e.g., Chikungunya, Mayaro, Ross River, Barmah Forest, O’nyong-nyong, and Sindbis viruses).
Preliminary diagnosis is based on the patient’s clinical features, places and dates of travel, and activities. Laboratory diagnosis is generally accomplished by testing serum or plasma to detect virus, viral nucleic acid, or virus-specific immunoglobulin M and neutralizing antibodies. Click for more information about diagnostic testing.
Although Zika virus disease is not nationally reportable in the United States, healthcare providers are encouraged to report suspected cases to their state or local health departments to facilitate diagnosis and mitigate the risk of local transmission. State health departments are encouraged to report laboratory-confirmed cases to CDC through ArboNET, the national surveillance system for arboviral disease.
Treatment
No specific antiviral treatment is available for Zika virus disease. Treatment of symptoms may include rest, fluids, antipyretics, and analgesics. Aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided until dengue can be ruled out to reduce the risk of hemorrhage.
For Health Care Providers: Diagnostic Testing
During the first week after onset of symptoms, Zika virus disease can often be diagnosed by performing reverse transcriptase-polymerase chain reaction (RT-PCR) on serum. Virus-specific IgM and neutralizing antibodies typically develop toward the end of the first week of illness; cross-reaction with related flaviviruses (e.g., dengue and West Nile viruses) is common and may be difficult to discern. Plaque-reduction neutralization testing can be performed to measure virus-specific neutralizing antibodies and discriminate between cross-reacting antibodies in primary flavivirus infections.
Zika virus testing is performed at the CDC Arbovirus Diagnostic Laboratory. Contact your state health department to facilitate testing.
Please refer to the instructions for sending diagnostic specimens to CDC, which also includes detailed instructions for completing the CDC specimen submission form 50.34[PDF - 2 pages]. Please note: Because Zika virus testing is not listed in the drop-down menu for the Test Order Name field of form 50.34 (located on 1st page, top left), you will need to select “ARBOVIRUS SEROLOGY” and then type “Zika testing” in the Brief Clinical Summary field located at the top of the second page of the form.
Test results are normally available 4 to 14 days after specimen receipt. Reporting times for test results may be longer during summer months when arbovirus activity increases. Receipt of a hard copy of the results will take at least 2 weeks after testing is completed.



